In recent years, the global awareness of Mpox has grown significantly, yet many in the Philippines remain unaware of the specific risk factors associated with the disease. Understanding Mpox risk factors is crucial for preventing its spread and safeguarding health, particularly for those most vulnerable. This comprehensive guide will walk you through the risk factors, the demographic most at risk, and measures to mitigate these risks effectively.
Understanding Mpox

Monkeypox is a viral zoonotic disease that poses a significant threat to public health. Its elusive nature and rapid spread make it difficult to control, particularly in countries like the Philippines where specific risk factors contribute to its prevalence. By understanding the history and implications of monkeypox, we can work towards effective strategies for prevention and control.
History of Mpox and Its Impact on Today’s Health
Monkeypox is a serious illness in the same family as the smallpox virus. The monkeypox virus primarily affects wild animals, particularly rodents and monkeys, which occurred in 1958 when experts first discovered the illness. However, in 1970, the first human case of monkeypox was reported in the Democratic Republic of the Congo (DRC). Since then, sporadic outbreaks have occurred in several African countries.
Unfortunately, these outbreaks have not been localized and contained within rural areas. In 2022, after the COVID cases, a global outbreak of Mpox shook several countries. The rapid spread of monkeypox is a cause for concern because cases of Mpox in West Africa and Central Africa lead to severe illness and even death. These scenarios are some of the reasons why people should know the Mpox risk factors. Thus, allowing them to strengthen their immune system and protect their overall well-being.
Signs of Mpox Occurrence: Recognizing the Telltale Symptoms
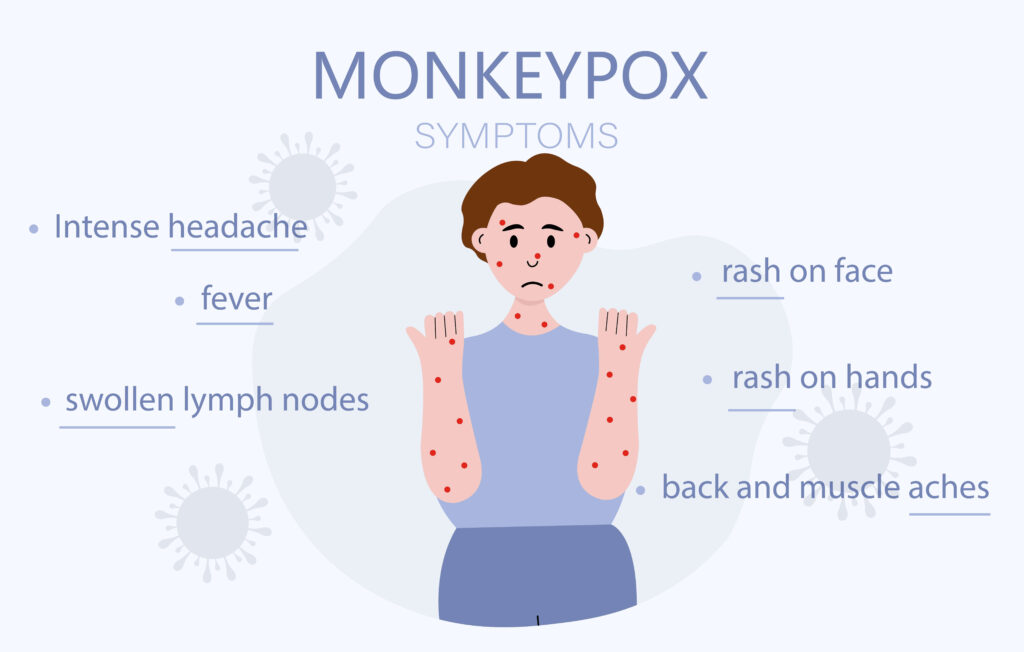
The enigmatic nature of this illness manifests through a range of distinctive symptoms of Mpox that set it apart from common diseases. Recognizing these signs is crucial for swift intervention and effective management of Mpox cases, shedding light on their unpredictable nature and the importance of vigilance in healthcare practices.
Unexplained Rashes
One of the early signs of Mpox is the sudden appearance of unexplained rashes on the skin. These rashes may be itchy and red, and may spread rapidly. They can appear anywhere on the body and may be mistaken for other common skin conditions. The rashes can turn into painful skin lesions during their occurrence. It’s best to not scratch or pop them as it can intensify the pain leading to discomfort until recovery.
Recurring Fevers
Another characteristic symptom of Mpox is recurring fevers that come and go without any apparent cause. These fevers may be accompanied by other flu-like symptoms such as headache, body aches, and fatigue.
Respiratory Symptoms
Mpox can also affect the respiratory system, leading to symptoms such as coughing, sneezing, sore throat, and difficulty breathing. These symptoms may be mild initially but can worsen over time.
Fatigue and Weakness
Many individuals with Mpox report feeling extreme fatigue and weakness that persists even after rest. This fatigue can significantly impact daily activities and may take weeks or even months to resolve.
Joint Pain and Muscle Aches
Joint pain and swelling are common in Mpox cases. This symptom can affect multiple joints in the body and may be mistaken for arthritis or other inflammatory conditions. Aside from that, patients with this illness may also experience pain in their muscles. These symptoms are similar to flu, which is why it’s best to seek immediate help to confirm Mpox occurrence.
Enlarged Lymph Nodes
Swollen lymph nodes are often observed in Mpox cases. These swollen nodes may be tender to touch and can be found in various areas of the body, such as the neck, armpits, and groin.
It is important to note that these symptoms may vary from person to person, and not all individuals with Mpox will experience all of these signs. If you or someone you know is experiencing any of these symptoms, it is crucial to seek medical attention for proper diagnosis and management.
Population Groups High Risk for Monkeypox
Individuals with Weakened Immune Systems
Newborn infants whose immune system is not built yet can be vulnerable to the threat of the Monkeypox virus. It can occur if the mother is infected and tries to nurse the infant, despite the Mpox symptoms occurring. Aside from that, people with compromised immune systems, such as HIV/AIDS patients, are at a heightened risk due to their reduced ability to fight infections.
Healthcare Workers
On the other hand, healthcare practitioners like doctors, nurses, etc. are the first line when it comes to helping patients to recover. Unfortunately, it also opens the possibility for them to get infected when their immune system is down. In that case, respiratory droplets from patients or even skin contact with them can be a potential threat.
Traveling Individuals
Moreover, individuals who have a travel history to either local or international places where the Monkeypox virus thrives can be more prone to contracting this severe disease. If such a situation occurs, it’s best to consult a health expert for risk assessment.
Urban Poor Communities
Lastly, crowded living conditions can accelerate the spread of infectious diseases like Mpox, making the urban poor particularly susceptible. This community setting can be alarming, especially if preventive initiatives are lacking. Thus, resulting in a possible chance of Mpox widespread.
Risk Factors for Mpox in the Philippines
In the Philippines, several risk factors contribute to the prevalence of monkeypox. The country has a high population density, which increases the likelihood of person-to-person transmission. Aside from that, there are still other factors that can be indicated as Mpox risk factors.
Let’s discuss each of the Mpox risk factors below!
Lifestyle and Health Mpox Risk Factors
Mpox Risk Factors: Cultural and Behavioral Factors
Traditional Practices
Certain cultural or traditional practices that involve close physical contact, such as hugging, kissing, or handshaking, can also pose risks for the transmission of infectious diseases like smallpox. It is important to be mindful of these practices and consider alternative ways to show affection or respect to prevent the spread of illness.
Stigma and Misinformation
Meanwhile, lack of information about Mpox can be a cause for more cases of Mpox. Without such knowledge can result in people being too lax about the situation. At the same time, it can also be a reason for stigma against Mpox patients due to a lack of understanding of its effect on the patient’s health.
Healthcare professionals, community leaders, and organizations need to work together to promote accurate information and provide support for those in need. By working together, we can create a more informed and supportive environment that encourages individuals to prioritize their health and well-being.
Mpox Risk Factors: Financial Aspect
Healthcare Costs
Dealing with severe illnesses like Mpox commonly includes the financial capacity of patients to pay for their recovery. Unfortunately, many Filipino families don’t have enough means for treatment, especially if severe cases are involved. In short, it can be one of the Mpox risk factors due to not seeking immediate treatment.
Mpox Risk Factors: Legal and Policy Considerations
Government Response and Policies
Another Mpox risk factor is the lack of policies and government response against the threat of Mpox. When the government agencies assigned to bid for the health systems decide poorly about such a threat, it can lead to more vulnerable groups in the population. In short, widespread Mpox can occur.
By taking proactive steps to address Mpox outbreaks, the government can significantly influence risk reduction and minimize the impact of the disease on the population. Additionally, these efforts can help to prevent the spread of Mpox and protect the overall health and well-being of the Filipino people.
Currently, the Philippine government addresses Mpox outbreaks through a combination of policies and public health initiatives. These measures include implementing public awareness and education about the disease, and improving healthcare plans to better respond to outbreaks.
Mpox Risk Factors: Psychological Impact of Mpox
Mental Health Concerns
In connection with the stigma against Mpox patients, individuals might become hesitant about seeking help due to this factor. At the same time, the Mpox virus itself can impact the psychological health of patients. Individuals can experience anxiety and stress related to the infection, which should be addressed through comprehensive health services.
Control Measures for Monkeypox

Vaccination and Immunization
It is important to have open and informed discussions about the availability and effectiveness of Mpox vaccines to provide a significant layer of protection for at-risk populations. Unfortunately, this form of control measure is not available yet in the Philippines.
DOH remains firm in its decision to buy doses of vaccines against Mpox as part of its initiatives. However, other countries need more vaccines due to continuous Mpox cases. It’s best to wait for further announcements about the availability of the vaccine. That way, you and your family can receive the immunization.
Public Health Education
Public health education about Mpox is crucial for preventing more cases of Mpox. By increasing awareness and understanding of Mpox, individuals can take proactive measures to protect themselves and others from contracting the disease. This can ultimately lead to a decrease in transmission rates and contribute to the overall public health efforts to control and prevent the spread of Mpox.
There are infographics released by the DOH to help Filipinos understand Mpox and its nature clearly.
Technological Advances in Managing Mpox
Diagnostic Tools
Advancements in diagnostic technologies have the potential to greatly improve the early detection and containment of outbreaks. One such example is the polymerase chain reaction (PCR) test, which has been recommended by the World Health Organization for confirming patients with Mpox.
This test allows experts to quickly and accurately identify individuals who have been infected, enabling swift isolation and treatment to prevent further spread of the disease. By utilizing cutting-edge diagnostic tools, public health officials can more effectively respond to outbreaks and ultimately save lives.
Online Consultations
Mpox is a contagious condition, which means isolation is a great choice for individuals with Mpox. In that case, utilizing an online consultation platform is a convenient option to receive medical advice and prescriptions. It also promotes the reduction of risk of exposure to Mpox or other illnesses, which makes it an ideal option for a consultation.
By utilizing this option, patients can also access medical care from the comfort of their own homes, which is especially beneficial for those who may be immunocompromised or at higher risk for complications from Mpox. Overall, it offers a valuable tool in preventing the spread of Mpox while ensuring that patients still have access to necessary medical care.
Frequently Asked Questions
What are the complications of Mpox in the Philippines?
Complications of Mpox in the Philippines can include pneumonia, encephalitis, and severe dehydration. These complications can be life-threatening, especially in vulnerable populations. Furthermore, pregnant patients who get infected can also experience complications such as loss of the pregnancy.
That’s why if you think you might have Mpox, it’s best to think of your health and seek immediate help.
Can sexual contact potentially lead to Mpox?
While the Mpox virus can be transmitted through sexual activity, it doesn’t mean in general that all people will get Mpox. It can only occur if one of the people is already infected and passed it on to the other person. If your sexual partner developed Mpox symptoms, most likely you will develop them too.
Conclusion
There are several Mpox risk factors that people must consider to ensure protection against Mpox. Each of them can be a root cause for the spread of Mpox, not until people begin to recognize its impact. Last month, we already had a few confirmed cases, and this month, more cases appeared. It’s important to stay informed and prepared to reduce the risk of exposure to a contagious illness.
Contribute to the overall health security of the community by recognizing the risk factors. Book an online consultation with an infectious disease doctor for further assistance about Mpox.
Mpox Risk Factors Quiz
Test your knowledge about Mpox prevention
Explanation