Navigating the complexities of skin conditions can be daunting, especially when outbreaks like Monkeypox enter the mix. In the Philippines, distinguishing Mpox blisters from other rashes is crucial not only for effective treatment but also for preventing spread within communities. This detailed guide will empower you with the knowledge to identify Mpox symptoms accurately and manage them responsibly at home.
Introduction: Monkeypox Origin
Monkeypox or Mpox, the new preferred term, is a contagious illness that made its global outbreak in 2022. Before the global Mpox spread, the monkeypox first originated in Central and West Africa in 1958 The monkeypox virus was discovered on wild animals like monkeys. Later on, the first case of Mpox was documented in 1970 in the Democratic Republic of the Congo DRC. As of today, DRC continues to have the highest number of cases of Mpox with high death rates in all African countries.
Mpox Cases in the Philippines
As mentioned, Mpox became a public health threat not only in Africa but also in Europe and Asia. The Philippines is one of those countries in Asia that suffered from several Mpox outbreaks. It began in July 2022 and branched out to December 2023. However, more cases have risen from August to the present year.
According to the DOH, they have confirmed 8 active cases of Mpox, each with a visible Mpox symptom, Mpox blisters. The virus spreads among various cities, which puts people on heightened alert. Despite that, news outlets provide crucial information to keep everyone updated and to promote better care against the threat of Mpox.
Recently, they’ve discussed the plan to purchase Mpox vaccines and offer free polymerase chain reaction testing for people. DOH says these plans are ongoing due to a lack of alarming cases and the lack of resources.
Common Symptoms of Mpox
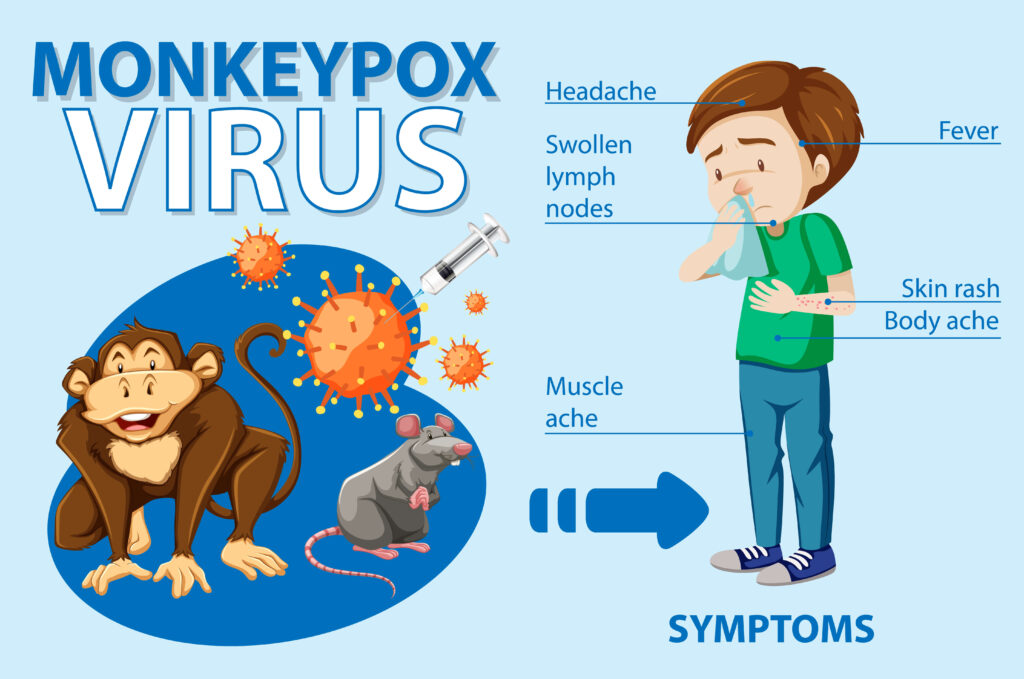
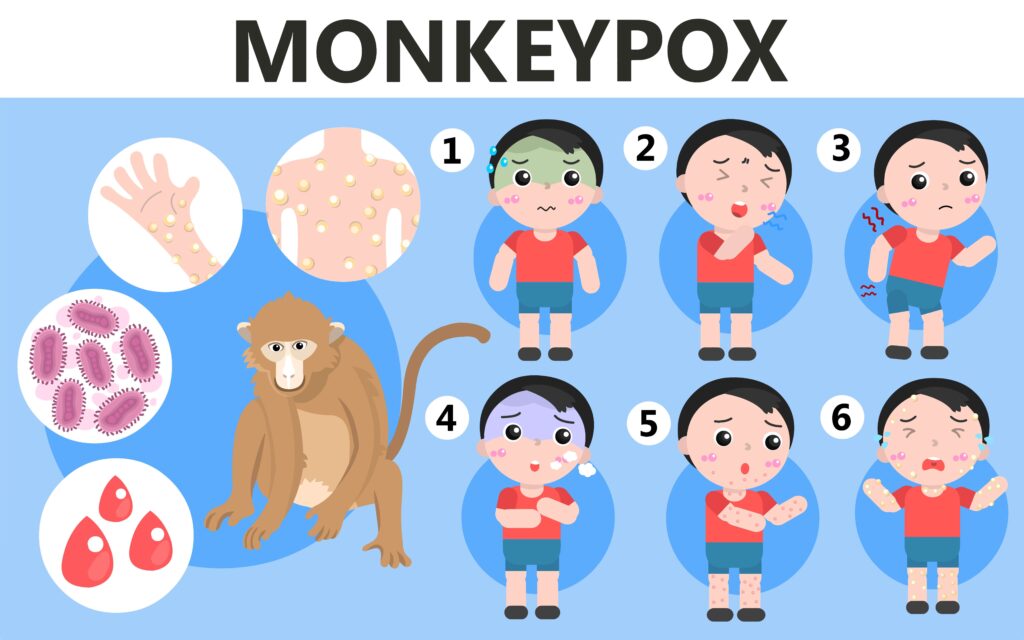
Aside from Mpox blisters, there are other signs to look out for when checking if the health is compromised by the Mpox virus. Here are some of the signs of Mpox people can refer to for individual risk assessment:
- swollen lymph nodes
- sore throat
- fever
- chills
- low energy
- muscle aches
If you might notice, these symptoms may be parallel with the flu. That’s why the indication of having Mpox can’t be determined immediately, especially if these symptoms appear first. However, when the rashes appear, there’s a high chance that the condition is related to Mpox.
What are Mpox Blisters?

As mentioned, these blisters are the hallmark of the disease. However, that’s not enough for an accurate diagnosis as other skin conditions also involve skin lesions. Still, that doesn’t mean that people can’t determine the difference between Mpox blisters from other pox-like skin conditions.
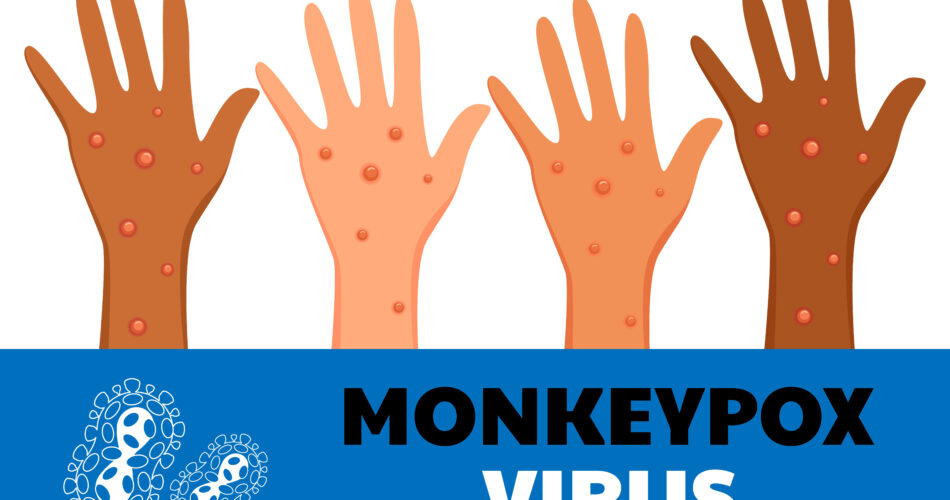
For instance, Mpox blisters are known to begin as flat hives, which grow into water-filled blisters. Furthermore, the Mpox blisters are deep-seated with dots on top. These Mpox blisters are found in various areas of the body.
Here are some of the known locations:
- soles of the feet
- palms of the hand
- chest
- anal region
- groin area
- private part of the body
Differentiating Mpox from Other Skin Conditions
| Type of Rash | Visual Comparison | When They Develop |
| Mpox Blisters | Big well-compact Mpox lesions, deep, pus-filled, and often painful | appear in waves |
| Chickenpox Rash | Smaller, itchier, and more superficial | appear at the same time |
| Herpes Rash | Grouped blisters that recur and are typically localized | appear in cluster |
It is easy to spot their differences, which can be shown in the table above. If this guide is still not enough, it’s best to visit a healthcare worker. That way, they can help determine if the blisters present are Mpox rash.
Impact of Mpox Blisters in Different Settings

If the lesions present are Mpox-related, it’s best to learn the proper health care to manage the Mpox blisters. At the same time, having this knowledge helps to avoid the risk of exposure for other people.
Monkeypox is a severe disease that can easily be transmitted through close contact and skin contact. For instance, a patient with Mpox blisters can transmit the virus through hugging, holding other people’s hands, kissing, and sexual contact. Additionally, taking face-to-face with an infected patient can also lead to transmission of Mpox virus.
On the other hand, indirect contact such as touching the belongings of the Mpox patient can also lead to getting infected. It is likely to happen at home. In that case, it’s highly important to know how to handle similar situations to properly manage Mpox, and prevent getting infected.
Effective Home Care Strategies

Due to the possible transmission threats, individuals with Mpox blisters and other Mpox symptoms are encouraged to isolate at home. Home space allows proper virus containment as the patient awaits recovery in 2 to 4 weeks.
During the recovery week, it is important to fulfill the following home care strategies to ensure healing. Let’s discuss them below!
Hygiene
One of the important aspects of home care is practicing proper hygiene. Due to the indirect transmission of Mpox, it is ideal to always wash one’s hands. At the same time, sanitizing surfaces and other parts of the house can help get rid of the virus. Thus, preventing Mpox spread.
Wound Care
On the other hand, patients with Mpox blisters must be aware of how to handle their lesions. Mpox rashes are deep lesions that can be painful when popped. When that happens, wash the area with water and mild soap, then dry with a clean towel. It is possible to develop a bacterial infection, so it’s best to use an antiseptic to dress the popped Mpox lesions.
Bacterial infection is a possible complication of this serious illness. To address this problem better, it’s best to seek help from a doctor. That way, you can know what type of antiseptic medicine to use for the wound.
Avoiding Intimate Acts
One of the higher risks of more serious Mpox disease is getting involved with an Mpox patient. Whether it is hugging, kissing, or sexual contact, these practices can all result in Mpox transmission. That’s why it is best to avoid participating in sexual activities with your partners.
When to Consult a Healthcare Provider
- Worsening Condition: Increasing pain or signs of secondary infection.
- Respiratory Symptoms: Development of coughing or shortness of breath.
Frequently Asked Questions
Are Mpox blisters contagious?
Yes, they are contagious until they have fully crusted over, healed, and revealed a new layer of skin. In that case, it is important to not scratch the blisters and perform close physical contact.
How long do Mpox blisters last?
The healing process usually spans 2-4 weeks, during which the blisters scab over and fall off.
What is severe Mpox?
According to the World Health Organization, severe Mpox may involve larger lesions that can grow on the genitals, eyes, and even the mouth area. People with immune suppression can develop severe Mpox and may suffer from organ complications.
Conclusion
Recognizing and managing Mpox blisters effectively requires an informed approach. By understanding the specifics of these symptoms and implementing recommended practices, Filipinos can mitigate the impact of Mpox and protect themselves, and their families.
Take a leap and regain control of your health despite the rising cases of Mpox. Book an online consultation with an infectious disease doctor when needed.
Mpox Blisters Quiz
Test your knowledge about Mpox symptoms and prevention