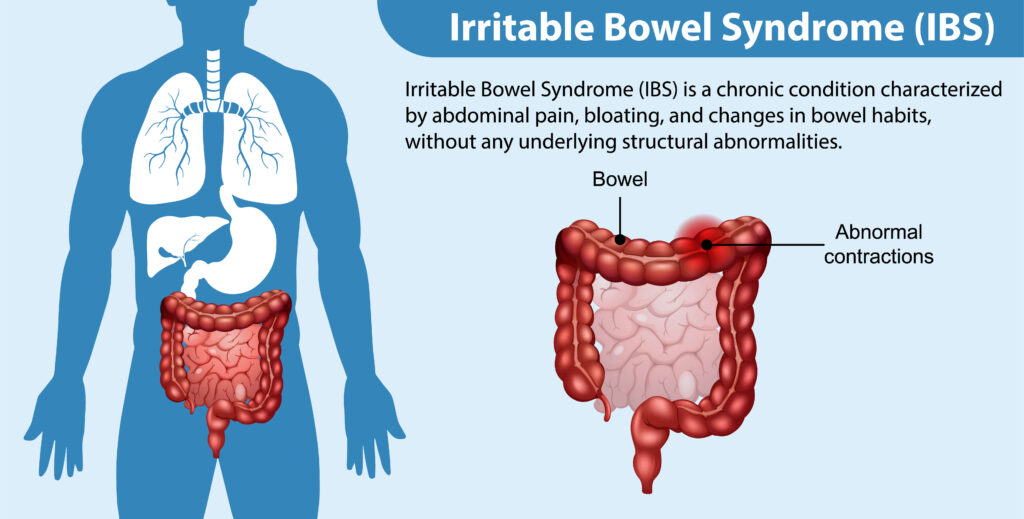
Irritable bowel syndrome (IBS) is a common gastrointestinal disorder that affects a significant portion of the population. It is characterized by recurring abdominal pain, discomfort, and changes in bowel movements. While the exact cause of IBS is not yet fully understood, researchers have identified several factors that may contribute to its onset. In this article, we will explore the various causes of IBS and their potential impact on individuals.

Understanding Irritable Bowel Syndrome
Before delving into the factors behind the onset of IBS, it is essential to have a basic understanding of this condition. IBS is a functional disorder, meaning that it affects the normal functioning of the digestive system without causing any structural changes. It is often diagnosed based on specific symptoms and the exclusion of other gastrointestinal conditions.
However, the impact of IBS goes beyond its classification as a functional disorder. It is a condition that can significantly affect the quality of life for those who experience its symptoms. The physical discomfort and pain associated with IBS can be debilitating, making it difficult for individuals to engage in their daily activities and enjoy a normal lifestyle.
Defining IBS: A Brief Overview
IBS is characterized by a variety of symptoms, including abdominal pain or discomfort, bloating, and changes in bowel habits. These changes can manifest as diarrhea, constipation, or both, often alternating between the two. The unpredictable nature of these symptoms can make it challenging for individuals with IBS to plan their day-to-day activities, as they never know when an episode may occur.
Furthermore, the severity of symptoms can vary from person to person. While some individuals may experience mild discomfort, others may face intense pain that disrupts their daily lives. This variability in symptom severity adds to the complexity of managing and treating IBS.
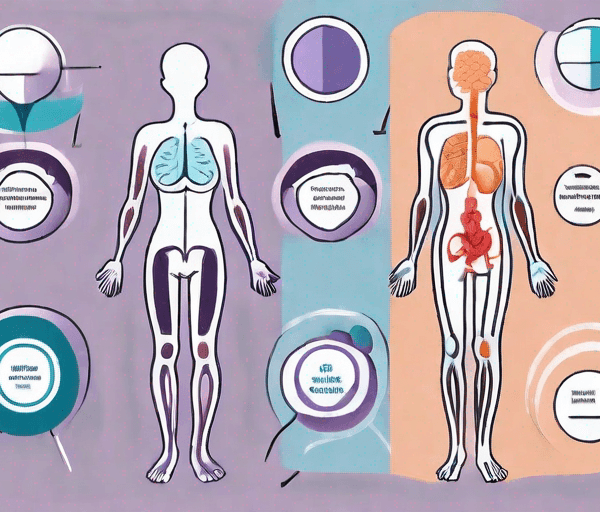
Symptoms Associated with IBS
While the hallmark symptoms of IBS are related to the digestive system, the condition can also cause non-gastrointestinal symptoms. These may include fatigue, headache, backache, and sleep disturbances. The presence of these additional symptoms can further complicate the diagnosis and management of IBS.
Moreover, the psychological impact of IBS should not be overlooked. Many individuals with IBS report experiencing anxiety and depression. The constant worry about when the next episode will occur and the fear of embarrassment in social situations can take a toll on a person’s mental well-being.
It is important to note that IBS is a chronic condition, meaning that it is long-lasting and requires ongoing management. While there is no cure for IBS, there are various treatment options available to help individuals alleviate their symptoms and improve their quality of life. These may include dietary modifications, stress management techniques, and medications.
Overall, understanding the complexities of IBS is crucial in order to provide appropriate support and care for individuals living with this condition. By expanding our knowledge and awareness, we can work towards creating a more compassionate and inclusive society for those affected by IBS.

The Role of Genetics in IBS
Research suggests that genetic factors may play a role in the development of Irritable Bowel Syndrome (IBS). Family studies have shown a higher prevalence of IBS among first-degree relatives of affected individuals, indicating that there may be a hereditary component to the condition.
However, it is important to note that genetics is just one piece of the puzzle when it comes to understanding IBS. Environmental factors, such as diet, stress, and gut microbiota, also play a significant role in the development and progression of the condition.
Hereditary Factors and IBS
Certain genetic variations have been associated with an increased risk of developing IBS. For example, a study identified a gene called SLC6A4 that is involved in serotonin transportation. Serotonin is a neurotransmitter that regulates various bodily functions, including gastrointestinal motility. Variations in this gene have been linked to alterations in serotonin levels and an increased susceptibility to IBS.
Another gene that has been implicated in IBS is the TPH1 gene, which encodes for an enzyme involved in the production of serotonin. Variations in this gene have been associated with altered serotonin synthesis, potentially affecting gut motility and sensitivity.
While these genetic variations may increase the risk of developing IBS, it is important to remember that they do not guarantee the development of the condition. Many individuals with these genetic variations never develop IBS, highlighting the complex interplay between genetics and other factors.
Genetic Mutations and IBS
In addition to hereditary factors, genetic mutations may also contribute to the development of IBS. Mutations in certain genes involved in gut barrier function and immune system regulation have been identified in individuals with IBS.
One such gene is the NOD2 gene, which plays a crucial role in the innate immune response. Mutations in this gene have been associated with an increased risk of developing IBS, possibly due to abnormal immune responses in the gut.
Furthermore, mutations in genes involved in the regulation of tight junction proteins, which are responsible for maintaining the integrity of the gut barrier, have also been linked to IBS. Disruptions in the gut barrier can lead to increased intestinal permeability, allowing harmful substances to enter the bloodstream and trigger inflammation and IBS symptoms.
It is worth noting that the presence of these genetic mutations does not guarantee the development of IBS. The interplay between genetic predisposition and environmental factors is still not fully understood and requires further research.
In conclusion, while genetics certainly play a role in the development of IBS, it is a complex condition influenced by a variety of factors. Further research is needed to fully understand the genetic mechanisms underlying IBS and how they interact with environmental factors.
Dietary Triggers of IBS
Another factor that has been implicated in the onset of IBS is diet. Certain foods and dietary habits can exacerbate symptoms and contribute to the development of the condition.
IBS, or Irritable Bowel Syndrome, is a chronic gastrointestinal disorder that affects millions of people worldwide. It is characterized by symptoms such as abdominal pain, bloating, diarrhea, and constipation. While the exact cause of IBS is unknown, research suggests that diet plays a significant role in triggering and managing symptoms.
Common Food Irritants
Several types of food have been known to trigger symptoms in individuals with IBS. These include fatty foods, spicy foods, alcohol, caffeine, and foods high in fructose or lactose. Fatty foods, such as fried and greasy dishes, can be difficult to digest and may lead to bloating and discomfort. Spicy foods, on the other hand, can irritate the digestive system and cause abdominal pain. Alcohol and caffeine are known to stimulate the gut and can worsen symptoms in some individuals. Foods high in fructose or lactose, such as certain fruits, vegetables, and dairy products, can be poorly absorbed by the body and may trigger diarrhea, gas, and bloating.
It is important for individuals with IBS to identify their personal trigger foods and avoid consuming them to minimize symptoms. Keeping a food diary and noting any symptoms that occur after eating can help in identifying specific trigger foods. Once identified, these foods can be eliminated or reduced from the diet to alleviate symptoms and improve overall quality of life.
The Impact of Dietary Habits on IBS
Alongside specific trigger foods, dietary habits can also influence the development and severity of IBS symptoms. Irregular meal patterns, skipping meals, and eating too quickly can all disrupt the digestive process and contribute to gastrointestinal distress. When meals are skipped or eaten irregularly, the digestive system may become imbalanced, leading to symptoms such as bloating, constipation, or diarrhea. Eating too quickly can also lead to swallowing air, which can cause bloating and discomfort.
Adopting a healthy and regular eating routine can help manage symptoms and improve overall digestive health. It is recommended to eat small, frequent meals throughout the day, rather than three large meals. This helps to keep the digestive system functioning smoothly and prevents overloading the gut. Chewing food thoroughly and eating slowly can also aid in digestion and reduce the risk of bloating and discomfort.
In addition to meal patterns, it is important to pay attention to portion sizes and the types of foods consumed. Including a variety of fruits, vegetables, whole grains, and lean proteins in the diet can provide essential nutrients and promote a healthy gut. Drinking an adequate amount of water and staying hydrated is also crucial for maintaining proper digestion and preventing constipation.
Overall, understanding the role of diet in IBS and making appropriate dietary changes can significantly improve symptoms and enhance the quality of life for individuals with this condition. Working with a healthcare professional or registered dietitian can provide personalized guidance and support in managing IBS through diet.
Psychological Factors Contributing to IBS
Psychological factors, such as stress, anxiety, and depression, are closely linked to IBS. These factors can both contribute to the development of the condition and exacerbate existing symptoms.
IBS, or Irritable Bowel Syndrome, is a chronic gastrointestinal disorder that affects millions of people worldwide. It is characterized by abdominal pain, bloating, and changes in bowel habits. While the exact cause of IBS is unknown, research has shown that psychological factors play a significant role in its development and progression.
Stress and IBS
Stress is known to affect the gastrointestinal system, causing alterations in gut motility and sensitivity. When a person experiences stress, the body releases stress hormones, such as cortisol, which can disrupt the normal functioning of the digestive system. This can lead to symptoms commonly associated with IBS, such as diarrhea, constipation, and abdominal discomfort.
Chronic stress, whether it is related to work, relationships, or other life events, can increase the risk of developing IBS. Additionally, for individuals already diagnosed with the condition, stress can worsen symptoms and trigger flare-ups. It is essential for individuals with IBS to learn effective stress management techniques to help alleviate symptoms and improve overall well-being.
There are various stress management techniques that can be beneficial for individuals with IBS. These include relaxation exercises, such as deep breathing, meditation, and yoga. Engaging in regular physical activity, getting enough sleep, and maintaining a healthy diet can also help reduce stress levels and improve IBS symptoms.
Anxiety, Depression, and IBS
Anxiety and depression commonly coexist with IBS, and the relationship between these conditions is complex. It is unclear whether anxiety and depression are risk factors for IBS or if they develop as a result of living with the condition. However, research has shown that individuals with IBS are more likely to experience symptoms of anxiety and depression compared to those without the condition.
Living with a chronic condition like IBS can be challenging and can significantly impact a person’s mental health. The unpredictable nature of IBS symptoms, the social stigma associated with the condition, and the impact it can have on daily life activities can contribute to feelings of anxiety and depression.
Managing mental health is crucial for individuals with IBS. Therapy, such as cognitive-behavioral therapy (CBT), can help individuals develop coping mechanisms and address any negative thought patterns associated with the condition. Medications, such as antidepressants or anti-anxiety medications, may also be prescribed to help manage symptoms of anxiety and depression.
In addition to therapy and medications, there are other interventions that can significantly improve IBS symptoms and mental well-being. These include practicing self-care activities, engaging in hobbies and activities that bring joy, and seeking support from friends, family, or support groups.
It is important for individuals with IBS to prioritize their mental health and seek appropriate support and treatment. By addressing psychological factors, such as stress, anxiety, and depression, individuals can better manage their IBS symptoms and improve their overall quality of life.

Gut Microbiota and IBS
The gut microbiota, the complex community of microorganisms residing in the digestive tract, is increasingly recognized as a potential factor in the development of IBS.
The Importance of Gut Health
A healthy gut microbiota is crucial for maintaining proper digestive function and overall well-being. Imbalances in the gut microbiota, known as dysbiosis, have been observed in individuals with IBS. These imbalances can lead to increased inflammation, altered gut motility, and abnormal communication between the gut and brain.
Dysbiosis and its Role in IBS
Emerging research suggests that dysbiosis may contribute to the development and exacerbation of IBS symptoms. Imbalances in specific bacterial species and an overall reduction in microbial diversity have been observed in individuals with IBS. Targeted interventions, such as probiotics and dietary modifications, may help restore a healthy gut microbiota and alleviate symptoms.
In conclusion, while the exact causes of IBS remain elusive, various factors can contribute to its onset. Genetic predisposition, dietary triggers, psychological factors, and disruptions in gut microbiota all play a role in the development and exacerbation of IBS symptoms. By understanding these factors, individuals with IBS and healthcare professionals can work together to manage symptoms and improve overall quality of life.
Consulting with Your Doctor
If you’ve been experiencing the often debilitating symptoms of Irritable Bowel Syndrome, it’s essential to remember that you don’t have to face this challenging condition alone. While understanding the potential causes and triggers of IBS is a crucial step in managing it, seeking professional help from a healthcare provider is equally important. Don’t suffer in silence or resort to self-medication, as individual experiences with IBS can vary greatly, and what works for one person may not work for another. Your doctor can provide you with personalized guidance, tailored treatment options, and valuable insights to help you regain control of your digestive health and overall well-being.
Remember, taking that step to book and consult a doctor can be the first crucial step towards a happier, healthier life, free from the limitations IBS can impose. Your journey to better digestive health begins with seeking the right support and care, so don’t hesitate to reach out today. Your well-being is worth it. Book with your doctor today by clicking here.
🧠 Test Your IBS Knowledge
Learn more about the causes and factors behind Irritable Bowel Syndrome