Generally, blood pressure needs to be controlled if it exceeds the normal blood pressure range. However, if the systolic remains the same, and the diastolic blood pressure changes, there might be an underlying factor that patients must address. In that case, it is vital to know how to lower diastolic blood pressure effectively.
For today’s blog, we’ll take a deeper dive into understanding how and why you should lower your diastolic blood pressure. Let’s begin!
Understanding Blood Pressure Reading
There are two important numbers in reading your blood pressure results. Systolic blood pressure is the first number that indicates the power exerted on blood vessels when the heart beats to pump out blood to the circulatory system. The diastolic blood pressure is the second number that indicates the power exerted when the heart is resting between beats. For instance, 110/70 bp is a measurement of 110 systolic and 70 diastolic. This reading uses the mm Hg or millimeters of mercury for the unit measurement.
Normal blood pressure ranges from a systolic blood pressure reading of 110-130 mm Hg and a diastolic blood pressure reading of 60-70 mm Hg. Hence, an increase in normal blood pressure with a range of 130 to 139 mm Hg systolic pressure reading and 80 to 89 mm Hg diastolic pressure reading is categorized as high blood pressure also known as hypertension.
Different blood pressure readings can be observed throughout the day that are influenced by various activities and food intake.
What is High Diastolic Blood Pressure?
A high diastolic blood pressure is an illness related to hypertension. It is a type of high blood pressure wherein there’s a constant pressure in the arteries when the heart is at rest.
This scenario is alarming as it puts people at risk of stroke, heart attack, etc. In such cases, it’s best to seek professional help immediately to address this concern.
Risk Factors for High Diastolic Blood Pressure
Some common uncontrollable risk factors include age, cardiovascular diseases, and kidney disease.
Risk Factors for High Diastolic Blood Pressure
High diastolic blood pressure can be influenced by various factors, with some being particularly significant. Let’s explore three key risk factors in detail:
Age
The relationship between age and diastolic blood pressure is complex. While systolic blood pressure typically increases with age, diastolic blood pressure often follows a different pattern. People under 50 are more likely to have elevated diastolic blood pressure, which can be particularly concerning.
This occurs because younger arteries tend to be more resistant to blood flow, creating higher pressure when the heart is at rest. However, as we age, our arteries naturally become less elastic, which can actually lead to a decline in diastolic pressure while systolic pressure rises.
Cardiovascular Illness
Pre-existing cardiovascular conditions significantly impact diastolic blood pressure. Let’s discuss these conditions below:
- Atherosclerosis (hardening of arteries): It can cause increased resistance in blood vessels, leading to elevated diastolic pressure.
- Aortic valve issues: A condition that can also affect how blood flows through the heart and vessels, potentially raising diastolic pressure.
- Other conditions affecting heart muscle function: This can alter the heart’s ability to maintain normal pressure patterns between beats, further contributing to diastolic hypertension.
Kidney Disease
Lastly, the kidneys play a crucial role in blood pressure regulation, making kidney disease a major risk factor for diastolic hypertension. When kidneys are damaged or functioning improperly, they may fail to effectively filter excess fluid and sodium from the blood. This leads to fluid retention and increased blood volume, directly affecting diastolic pressure.
Meanwhile, a chronic kidney disease can also activate the renin-angiotensin-aldosterone system, a hormone cascade that raises blood pressure. Such kidney disease often causes arterial stiffness, which can contribute to sustained elevated diastolic pressure.
These risk factors often interplay with each other, potentially creating a cycle that can worsen blood pressure control. Regular medical monitoring and appropriate lifestyle modifications are essential for managing these risks effectively.
Diagnosis and Symptoms
The diagnosis of lower diastolic blood pressure is mainly based on a blood pressure reading of <130 mmHg/ ≥80 mmHg) accompanied by hypertensive symptoms. Patient-centered factors like age, weight, and medical comorbidities also play a significant part in patient diagnosis.
Following symptoms are observed in high diastolic pressure readings:
- Lightheadedness or dizziness
- Headache
- Increased sweating
- Heart palpitations
- Nausea or feeling like you are about to vomit
- Blurry vision
How to Lower Diastolic Blood Pressure?
Lifestyle changes and possible pharmacological treatment are beneficial in the management of high diastolic blood pressure. According to a study, most patients with high diastolic bp were younger people, have a high body mass index (BMI), and are smokers.
Hence, being fit, following a prescribed diet, proper exercise training, and quitting smoking are some efficient blood pressure management treatments. If lifestyle changes and diet changes are not enough to lower your blood pressure, your doctor may prescribe the following medications:
- Thiazide diuretics
- Angiotensin converting enzyme inhibitors (ACE)
- Angiotensin II receptor blockers (ARBs)
- Calcium channel blockers (CCB)
Note that most patients have existing maintenance medications for other existing medical conditions. It is important to check for drug-drug interactions when adding an antihypertensive drug to the patient’s treatment regimen. Also, watch out for a sudden drop in blood pressure when given these types of medication.
How to lower diastolic blood pressure naturally?

Here are 5 beneficial tips to achieve normal blood pressure naturally:
Maintain an Active Lifestyle (increase in aerobic exercises)
Physical exercise reduces blood pressure on exertion and is generally recommended regularly. It was observed that endurance training, resistance training, isometric, and combined training markedly decreased diastolic blood pressure. Shorter endurance training exercise duration at moderate to high intensity was noted to have larger blood pressure reductions.
Proper Diet for Weight Reduction
Long-term compliance with the DASH diet would help in reducing weight. Thus, leading to a decrease in blood pressure.
Stress Reduction
As a reaction to stress, your body produces hormones that increase blood pressure. It is important to know your stress factors and avoid them. Practice deep breathing exercises to reduce stress.
Avoid Smoking
Nicotine content in cigarettes causes an increase in blood pressure. It will be beneficial to taper and stop smoking to prevent an increase in blood pressure.
What are The Best Foods to Eat for Lowering Diastolic Blood Pressure?
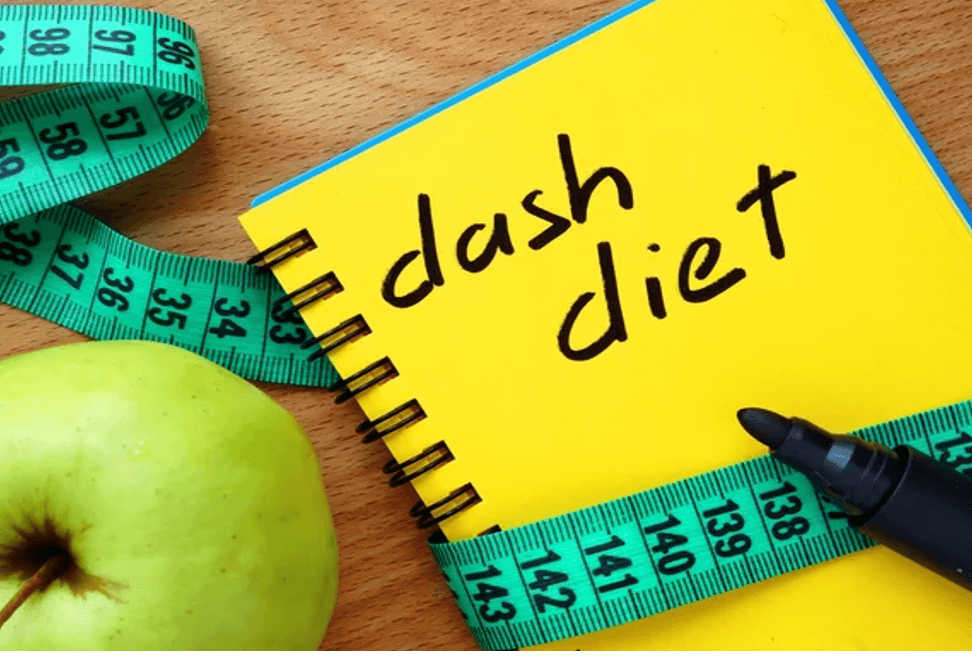
DASH Diet
Dietary Approaches to Stop Hypertension (DASH) diet is a suitable and effective nutritional diet strategy for a low blood pressure:
- Vegetables
- Fruits
- Fish
- Reduced portions of red meats
- Reduced sugar-sweetened foods
- Reduced sugar-sweetened beverages
- Low-fat dairy products
- Reduced saturated fat and cholesterol
Add Magnesium and Potassium-rich Food to Your Diet
Nuts, legumes, and vegetables contain magnesium which has a protective effect against hypertension. Potassium supplementation also showed to reduce blood pressure levels.
Consume High-fiber Food
Foods that are high in fiber such as whole oats, whole barley, legumes, peas, beans, and flax seeds are beneficial in patients with high blood pressure.
Probiotics
Studies reported the high efficacy of probiotics in reducing diastolic and systolic blood pressure in patients with underlying medical conditions such as diabetes and obesity.
Reduce Salt Intake
Since sodium can increase your blood pressure, reduce sodium intake to 1,500 milligrams or preferably less per day.
Reduce Alcohol Intake
Alcohol consumption elevates your blood pressure. It’s best to reduce your alcohol intake to lower your blood pressure to a normal range.
When to Consult with Your Doctor
High-risk patients with high blood pressure must have a routine check-up with their doctors.
Your doctor will lay out the best treatment plan that best suits your symptoms and condition. Also, consult with your doctor about a good BP monitor and some best practices for monitoring your blood pressure daily.
How to Book A Consultation with A Cardiologist
If you are in search of the best doctor for high blood pressure, using NowServing can be helpful. You can browse doctors located in Manila, Quezon City, Makati, Pasig, Taguig, and even doctors outside the Metro. Furthermore, you can also find doctors affiliated with prominent hospitals in this healthcare platform.
Here’s how to book a consultation:
- Click the link to view the list of cardiology doctors in the Philippines.
- Browse and select your preferred doctor by clicking the “Book Appointment” button.
- Choose if you are a new or old patient of the doctor
- Fill up the form with your information to finalize your appointment.
- Wait for the booking confirmation.
You can also use the NowServing app to book a consultation. Just download the app here.
Conclusion
Working on how to lower diastolic blood pressure can be challenging. There are several approaches on how to achieve the desired outcome. However, it is still best to follow a treatment plan that is specified for your situation. That’s why it is ideal to seek immediate help when a patient needs to lower diastolic blood pressure.
If you are one of those patients who needs to lower their diastolic blood pressure, don’t hesitate to book a consultation with a cardiologist.
References
Strandberg TE, Pitkala K. What is the most important component of blood pressure: systolic, diastolic or pulse pressure? Curr Opin Nephrol Hypertens. 2003 May;12(3):293-7. [PubMed]
Hoit BD. Pathophysiology of the Pericardium. Prog Cardiovasc Dis. 2017 Jan-Feb;59(4):341-348. [PubMed]
Kirshblum S, Eren F, Solinsky R, Gibbs K, Tam K, DeLuca R, Linsenmeyer T. Diastolic blood pressure changes during episodes of autonomic dysreflexia. J Spinal Cord Med. 2021 Sep;44(5):720-724. [PubMed]
Conell C, Flint AC, Ren X, Banki NM, Chan SL, Rao VA, Edwards NJ, Melles RB, Bhatt DL. Underdiagnosis of Isolated Systolic and Isolated Diastolic Hypertension. Am J Cardiol. 2021 Feb 15;141:56-61. [PubMed]
Li Y, Wei FF, Wang S, Cheng YB, Wang JG. Cardiovascular risks associated with diastolic blood pressure and isolated diastolic hypertension. Curr Hypertens Rep. 2014 Nov;16(11):489. [PubMed]
Alsaeed H, Metzger DL, Blydt-Hansen TD, Rodd C, Sharma A. Isolated diastolic high blood pressure: a distinct clinical phenotype in US children. Pediatr Res. 2021 Oct;90(4):903-909. [PubMed]
McEvoy JW, Daya N, Rahman F, Hoogeveen RC, Blumenthal RS, Shah AM, Ballantyne CM, Coresh J, Selvin E. Association of Isolated Diastolic Hypertension as Defined by the 2017 ACC/AHA Blood Pressure Guideline With Incident Cardiovascular Outcomes. JAMA. 2020 Jan 28;323(4):329-338. [PubMed]
Lee H, Yano Y, Cho SMJ, Park JH, Park S, Lloyd-Jones DM, Kim HC. Cardiovascular Risk of Isolated Systolic or Diastolic Hypertension in Young Adults. Circulation. 2020 Jun 2;141(22):1778-1786. [PubMed]
Sowers JR. Hypertension in the elderly. Am J Med. 1987 Jan 26;82(1B):1-8. [PubMed]
Dominguez L, Veronese N, Barbagallo M. Magnesium and Hypertension in Old Age. Nutrients. 2020 Dec 31;13(1):139. [PubMed]
Surampudi P, Enkhmaa B, Anuurad E, Berglund L. Lipid Lowering with Soluble Dietary Fiber. Curr Atheroscler Rep. 2016 Dec;18(12):75. [PubMed]
Dixon A, Robertson K, Yung A, Que M, Randall H, Wellalagodage D, Cox T, Robertson D, Chi C, Sun J. Efficacy of Probiotics in Patients of Cardiovascular Disease Risk: a Systematic Review and Meta-analysis. Curr Hypertens Rep. 2020 Aug 29;22(9):74. [PubMed]
Stabouli S, Papakatsika S, Kotsis V. Hypothyroidism and hypertension. Expert Rev Cardiovasc Ther. 2010 Nov;8(11):1559-65. [PubMed]
Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013 Feb 1;2(1):e004473. [PubMed]